Motor Delays: Early Identification and Evaluation
Information Source http://pediatrics.aappublications.org/Introduction
The American Academy of Pediatrics (AAP) recommends developmental surveillance at all preventive care visits and standardized developmental screening for motor delay of all children at ages 9, 18, and 30 months.1 Recently, developmental screening instruments and their clinical interpretations have emphasized the early detection of delays in language and social development, responsive to rising prevalence rates of autism spectrum disorders in US children.2 The most commonly used developmental screening instruments have not been validated on children with motor delays.3,4 Recognizing the equal importance of surveillance and screening for motor development in the medical home, this clinical report reviews the motor evaluation of children and offers guidelines to the pediatrician regarding an approach to children who demonstrate motor delays and variations in muscle tone. (This report is aimed at all pediatric primary care providers, including pediatricians, family physicians, nurse practitioners, and physician assistants. Generic terms, such as clinician and provider, are intended to encompass all pediatric primary care providers.)
Rationale for AAP findings
Gross motor development follows a predictable sequence, reflecting the functional head-to-toe maturation of the central nervous system. Although parents are reliable in reporting their child’s gross motor development,5,6 it is up to the clinician to use the parent’s report and his or her own observations to detect a possible motor delay.7
Gross motor delays are common and vary in severity and outcome. Some children with gross motor delays attain typical milestones at a later age. Other children have a permanent motor disability, such as cerebral palsy, which has a prevalence of 3.3 per 1000.8 Other children have developmental coordination disorder (DCD), which affects up to 6% of the population and generally becomes more evident when children enter kindergarten.9 When motor delays are pronounced and/or progressive, a specific neuromuscular disorder is more likely to be diagnosed. Motor delays may be the first or most obvious sign of a global developmental disorder. For infants, motor activities are manifestations of early development. It is often the case that children whose developmental trajectories are at risk may experience challenges in meeting early motor milestones. Establishing a specific diagnosis can inform prognostication, service planning, and monitoring for associated developmental and medical disorders. When the underlying etiology of motor delays is genetic, early recognition may assist parents with family planning. A timely diagnosis may reduce family stress related to diagnostic and prognostic uncertainties.5 For children with the few neuromuscular diseases for which treatments are available, outcomes may be improved when therapy is implemented early.10
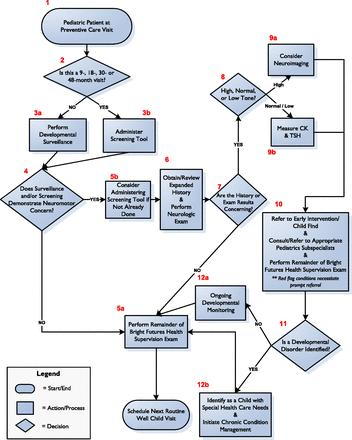
Focus groups were conducted with 49 pediatricians at the AAP National Conference and Exhibition in 2010, and members of the AAP Quality Improvement Innovation Network were surveyed to ascertain current provider practices and needs regarding neuromotor screening.11 Pediatricians described widely varying approaches to motor examinations and identification of delays and expressed uncertainty regarding their ability to detect, diagnose, and manage motor delays in children. Participants requested more education, training, and standardization of the evaluation process, including an algorithm to guide clinical care (Fig 1).